Cauda Equina Syndrome due to Lumbar Intervertebral disc herniation
What is cauda equina syndrome?
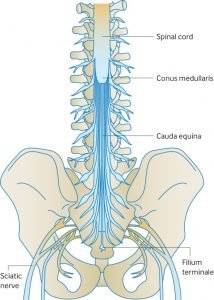
Schematic diagram showing Cauda Equina & Spinal Cord in Lumbar Spine
The collection of nerves at the end of the spinal cord is known as the cauda equina due to its resemblance to a horse’s tail. The individual nerve roots at the end of the spinal cord that provide motor and sensory function to the legs and the bladder continue along in the spinal canal. The cauda equina is the continuation of these nerve roots in the lumbar and sacral region. These nerves send and receive messages to and from the lower limbs and pelvic organs.
Cauda equina syndrome (CES) occurs when there is dysfunction of multiple lumbar and sacral nerve roots of the cauda equina. Most common cause of CES is a large herniated lumbar disc prolapse. Numerous other less common causes of cauda equina syndrome have been reported likes fractures and tumours.
Why it is an emergency?
An understanding of CES is important not only to orthopaedic surgeons and neurosurgeons but also to general practitioners, emergency department staff, and other specialists to whom these patients present. Recognition of the syndrome by all groups of clinicians is often delayed as it presents with impairment of bladder, bowel, and sexual function and perianal or ‘saddle’ numbness.
Patients with CES may experience some or all of these “red flag” symptoms.
- Urinary retention: the most common symptom. The patient’s bladder fills with urine, but the patient does not experience the normal sensation or urge to urinate.
- Urinary and/or fecal incontinence. The overfull bladder can result in incontinence of urine. Incontinence of stool can occur due to dysfunction of the anal sphincter.
- ‘’Saddle anesthesia” sensory disturbance, which involves the anus, genitals and buttock region.
- Weakness or paralysis of usually more than one nerve root affecting lower extremities.
- Pain in the back and/or legs (also known as sciatica).
- Sexual dysfunction.
If a patient is experiencing any of the “red flag” symptoms above, immediate medical attention is required to evaluate whether these symptoms represent CES.
What investigations to confirm the diagnosis?

MRI scan (sagittal view) showing large prolapsed disc at L5/S1 in a 34year old presenting with cauda equina syndrome (CES)
When CES is suspected a neurological examination of the legs should be performed, including perianal sensation and an assessment of anal tone. In most cases there is loss of perianal sensation. Magentic resonance imaging (MRI) is the imaging modality of choice. MRI is a diagnostic test that produces three-dimensional images of body structures using magnetic fields and computer technology.It shows soft tissues such as intervertebral disc, ligamentum flavum, dural sac, and nerve roots.
Is surgery the mainstay of treatment?
Recently published guidelines for the management of patients with back pain and neurological signs recommend urgent surgical referral to spine surgeon for suspected CES.
Surgery indicated is decompression at the level of the herniation, usually involving discectomy. The operation can be very demanding technically, and great care is needed to avoid causing further damage to nerve roots or tearing tightly compressed dura. When there is pressure on the cauda equina causing loss of sphincter control it would be understandable to think that the ideal treatment would be to remove the pressure as soon as possible with surgery.
Papers published suggest that intervention less than 48 hours after the onset of symptoms will produce a better outcome than intervention delayed for longer than 48hours. Even patients who undergo surgery after the 48-hour ideal time frame may experience improvement.
Requires long term rehabilitation
Many of these patients also require long term follow-up with rehabilitation medicine. Although short-term recovery of bladder function may lag behind reversal of lower extremity motor deficits, the function may continue to improve years after surgery. Following surgery, drug therapy coupled with intermittent self-catheterization can help lead to a slow, but steady, recovery of bladder and bowel function.
CES can affect people both physically and emotionally, particularly if it is chronic. People with CES may no longer be able to work, either because of severe pain, socially unacceptable incontinence problems, motor weakness and sensory loss – or a combination of these problems. Loss of bladder and bowel control can be extremely distressing and have a highly negative impact on social life, work and relationships. Patients with CES may develop frequent urinary infections. Sexual dysfunction can be devastating to the patient and his/her partner and may lead to relationship difficulties and depression. Sometimes severe nerve-type (neurogenic) pain may become chronic which will require prescription of pain medication with side effects that may cause further problems.
Many patients find that physical therapy and psychological counseling help them cope with problems faced after CES.
