The damaged joint is replaced with an implant that mimics the motion the natural joint and is made from combinations of metal, plastic and/or ceramic components.
The repla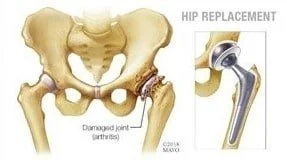 cement parts can be plastic (polyethylene), metal or ceramic and are used in different combinations:
cement parts can be plastic (polyethylene), metal or ceramic and are used in different combinations:
Best candidates: People with severe joint pain who haven’t been helped by other treatments. Hip replacement is most commonly recommended for severe osteoarthritis, but it’s sometimes used for inflammatory conditions such as rheumatoid arthritis or ankylosing spondylitis or for problems with development of the hip during childhood. Hip surgery may also be needed for fractures of the hip, including those resulting from osteoporosis. Improvement in implant durability means that TJR is more common in younger people than in the past.
Pros: Strong, proven track record for safety and success; reduces pain and improves mobility, daily functioning and quality of life.
Cons: All artificial joints can wear out, which may require joint revision surgery. Implants made entirely of metal (called metal-on-metal) can release metal ions that may damage bone and cause other health problems. Ask before surgery about an implant’s track record. TJR is not usually recommended for people who have weak bones or who are obese.
 The procedure involves cutting and removing bone or adding a wedge of bone near a damaged joint. In the knee, for example, an osteotomy shifts weight from an area damaged by arthritis to an undamaged area. In the hip it is often used to correct misalignment (hip dysplasia) that occurs early in life.
The procedure involves cutting and removing bone or adding a wedge of bone near a damaged joint. In the knee, for example, an osteotomy shifts weight from an area damaged by arthritis to an undamaged area. In the hip it is often used to correct misalignment (hip dysplasia) that occurs early in life.
Best candidates: Patients in their 30s and younger or who are too young for total joint replacement.
Pros: Can halt damage and delay the need for a joint replacement.
Cons: Osteotomies are not simple, warns Robert L. Barrack, MD, chief of staff for orthopaedic surgery at Barnes-Jewish Hospital in St. Louis. “Because the surgery is so complex and highly specialized, only a small percentage of surgeons are best suited to perform it.”
In people with inflammatory arthritis, the lining of the joints – the synovium – can become inflamed or grow too much, damaging surrounding cartilage and joints.In this procedure surgeons remove most or all of the affected synovium, either in a traditional, open surgery or by using arthroscopy.
Best candidates: People with limited cartilage damage in the affected area who have tried anti-inflammatory medications, but who continue to have inflammation or overgrowth of the synovium around the knee, elbow, wrist, fingers or hips.
Pros: Relieves pain and improves function, and people who have had the procedure may be able to reduce their dosage of anti-inflammatory drugs.
Cons: The procedure may limit range of motion and provide only temporary relief of symptoms.
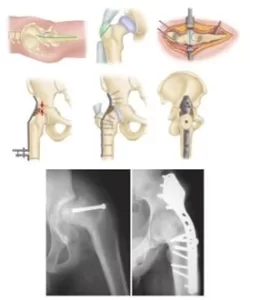 In this procedure surgeons use pins, plates, rods or other hardware to join two or more bones in the ankles, wrists, thumbs, fingers or spine, making one continuous joint. Over time the bones grow together and lock the joint in place.
In this procedure surgeons use pins, plates, rods or other hardware to join two or more bones in the ankles, wrists, thumbs, fingers or spine, making one continuous joint. Over time the bones grow together and lock the joint in place.
Best candidates: People with severe joint damage from OA or inflammatory arthritis.
Pros: This procedure is very durable, and results should last a lifetime.People who have weight-bearing joints fused can often take part safely in high-impact physical activity.
Cons: Fusing joints eliminates their motion and reduces flexibility. It also changes the joint’s normal biomechanics, which can put stress on surrounding joints and lead to the development of arthritis in other areas.
 An elective microsurgical procedure, free vascularized fibular grafting is an option for hip joint preservation.
An elective microsurgical procedure, free vascularized fibular grafting is an option for hip joint preservation.
Avascular necrosis (AVN) involves progressive necrosis of the hip provoked by vascular compromise of circulation to bone. The resulting bone death contributes to femoral head collapse and secondary osteoarthritis and is believed to be irreversible. The majority of patients with avascular necrosis are young, with an average age of 38 years.
Conditions and events known to contribute to AVN in bone include sickle cell disease, rheumatoid arthritis and other disease states, as well as trauma, alcohol abuse and prolonged corticosteroid use. Treatment options for mild-to-moderate AVN include core decompression and bone grafting.
For patients with late stage AVN, the standard treatment is total hip arthroplasty.
