Surgical management of patellar dislocations has evolved significantly over the last decade with advancement of biomechanical and anatomical knowledge of patellofemoral restraints and improved imaging techniques. Different surgical techniques have been described for its management but there is no consensus on its management modalities. Excessive lateral patellar mobility is seen after acute patellar dislocation.1,2 This is attributable to a medial retinacular injury, specifically of MPFL.3-6 In cadaveric studies, repair of medial patellofemoral ligament is necessary to restore lateral patellar mobility to within a normal range.3 With the knowledge of MPFL as a key restraint of lateral patellar translation, repair and reconstruction procedures to restore this medial constraint is of paramount importance in any procedure to stabilize the patella against subsequent patellar dislocations. How to best restore it is a matter of debate.
One prospective randomized study demonstrated equivalent results between operative and non operative management (Nikku et al 1997).7 Therefore, conservative management has become standard of care for initial treatment of first time patellar dislocations. Most procedures described to address patellar instability focus on the dynamic elements (muscles) that affect patellar forces and motion. Attention towards the passive medial restraints is a relatively new development. All the proponents of the medial patellofemoral repair and reconstruction share the common goal of restoring the medial stabilizer of patella. Management goals for the patients with first time patellar dislocation include restoration of normal pain free patellofemoral joint mechanics while minimizing the risk of recurrent subluxation and patella dislocation.
An arthroscopy should be performed if intra articular chondral damage is suspected. MRI may be useful to identify the location and degree of medial soft tissue injury preoperatively. Medial patellofemoral ligament injury with resultant laxity is a common feature among patients who experience recurrent patellar instability after patella dislocation.8 The restoration of a medial stabilizer by repairing and reconstructing the MPFL is a necessary component of all surgical procedures to correct lateral instability of patella. Whatever repair or reconstructive procedure is performed to prevent patella instability the injured ligament should be repaired or reconstructed to ensure a successful outcome (Fig 1).
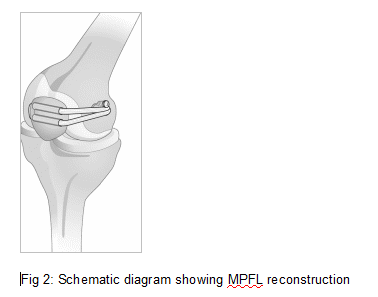
Many aspects of the reconstruction of the MPFL remain to be further examined such as tension, position, and location of fixation of the reconstructed MPFL (Fig 2). We should also investigate the material, length and volume of reconstructed material as well as resistance to rupture of the reconstructed MPFL. Additional research is needed to determine the optimal approach. A practical approach to surgery after patella dislocation is the minimal amount of surgery necessary to re-establish objective constraints of patella.
It would appear that the literature suggests that a MPFL reconstruction may provide favourable clinical and radiological outcomes for patients with patellar instability. However, a critical appraisal of the papers reviewed highlighted a number of methodological limitations which meant that any conclusions made from these papers should be interpreted with caution.